Laura López González, UC San Francisco

Alan Zambeli-Ljepovic, MD, MHS, sits at the arcade-like console like a church organist. He places his feet on the machine’s pedals and slips the middle finger and thumb of each hand into delicate pincher-like loops. The nearly six-foot-tall surgery robot beside him stirs to life in UC San Francisco’s Surgical Skills Lab.
From the console, Zambeli-Ljepovic, a surgery resident, controls the robotic system’s four massive arms: A flick of the wrist and a scalpel-laden limb makes a small incision into a liver, purchased for practice from the local butcher. A toe tap releases a buzz of cauterizing electricity from one of the arms.
Zambeli-Ljepovic relies on a robot arm-mounted camera to guide him. It is focused tightly on the operating table. He cannot see the robot’s four arms as they glide within millimeters of each other.
For that, there’s the lab director and surgery professor Hueylan Chern, MD. Today, the colorectal surgeon is providing one-on-one coaching to surgery residents.
“Think about what you’re going to use your static arm to set this incision up,” she cautions. “When I operate, I know almost every step I take before I take it: I know what my arm one is going to do, I know what the second arm is going to do.”

First robotic surgery assistant certification
Robotic-assisted surgery is booming in areas like urology, gynecology, and gastrointestinal procedures and is only expected to expand. Surgeries like these accounted for about 2.63 million procedures in the U.S. alone in 2024, a nearly 20% increase from 2023. The technology’s meteoric rise has been buoyed by its ability to allow surgeons to operate within extremely tight spaces, allowing for less invasive procedures and faster recoveries.
But robotic surgery training comes with challenges. For centuries, medical students have observed procedures standing at the operating table. But with robotic surgery, surgeons are enveloped by the console, away from the table. And they rely on a team of attending surgeons, nurses, scrub technicians, and bedside assistants, all of whom must share space around the table alongside a roughly 3-foot-wide robot. Medical students, Chern soon found, were crowded out.
“Learners are physically separated from the surgical team. We noticed that they weren’t really sure where they should be; sometimes we’d just see them sitting in the corner watching the video feed,” Chern explains. “They just didn’t feel engaged.”
To bridge the gap, Chern and UCSF medical students co-developed a first-of-its-kind program to certify final-year medical students as robotic bedside assistants, allowing them to safely participate in surgical cases. Once trained, bedside assistants position the robot before and after surgery, switch out arm-loaded medical equipment, and help ensure that the robot’s many arms maneuver safely past each other during procedures. The program offers medical students unparalleled exposure to the technology shaping the future of surgery, enhancing their competitiveness as candidates for prestigious residency programs.
The certification is the latest in UCSF’s nationally acclaimed robotic surgery training program. Created in 2018, the innovative teaching program spans the continuum from medical students to interns and residents. UCSF was one of the first in the West to perform robotic surgeries and, as of 2024, ranked among California’s busiest robotic surgery practices.
From the sidelines to the bedside
Surgical resident Anya Edwards, MD, MBA, remembers watching robotic surgery cases as a medical student at UCSF.
“Sometimes I wouldn’t even scrub in, I would just sit on the sidelines,” explains Edwards, who graduated in 2023. “I never felt integrated because I didn’t have a role.”
While still a student in 2021, Edwards collaborated with the Chern and Surgical Skills Lab to develop and pilot a medical student simulation curriculum that paired online and in-person training with the robot. School of Medicine Associate Dean Adnan Alseidi, MD, MEd, MBA; Research in Medical Education Director Patricia O’Sullivan, EdD, MS; and Associate Surgery Professor Shareef Syed, MD, helped design the program.
The 2021 project was a resounding success: nearly all participating students reported that it better prepared them for surgical rotations and entry into the surgical field, according to research Edwards co-authored with the faculty in 2023.
Edwards’ pilot became the foundation for UCSF’s robotic bedside assistant certification program, developed by Chern, O’Sullivan, as well as surgery residents and lab education fellows Camilla Gomes, MD, MSc and Alyssa Murillo, MD, MSc.
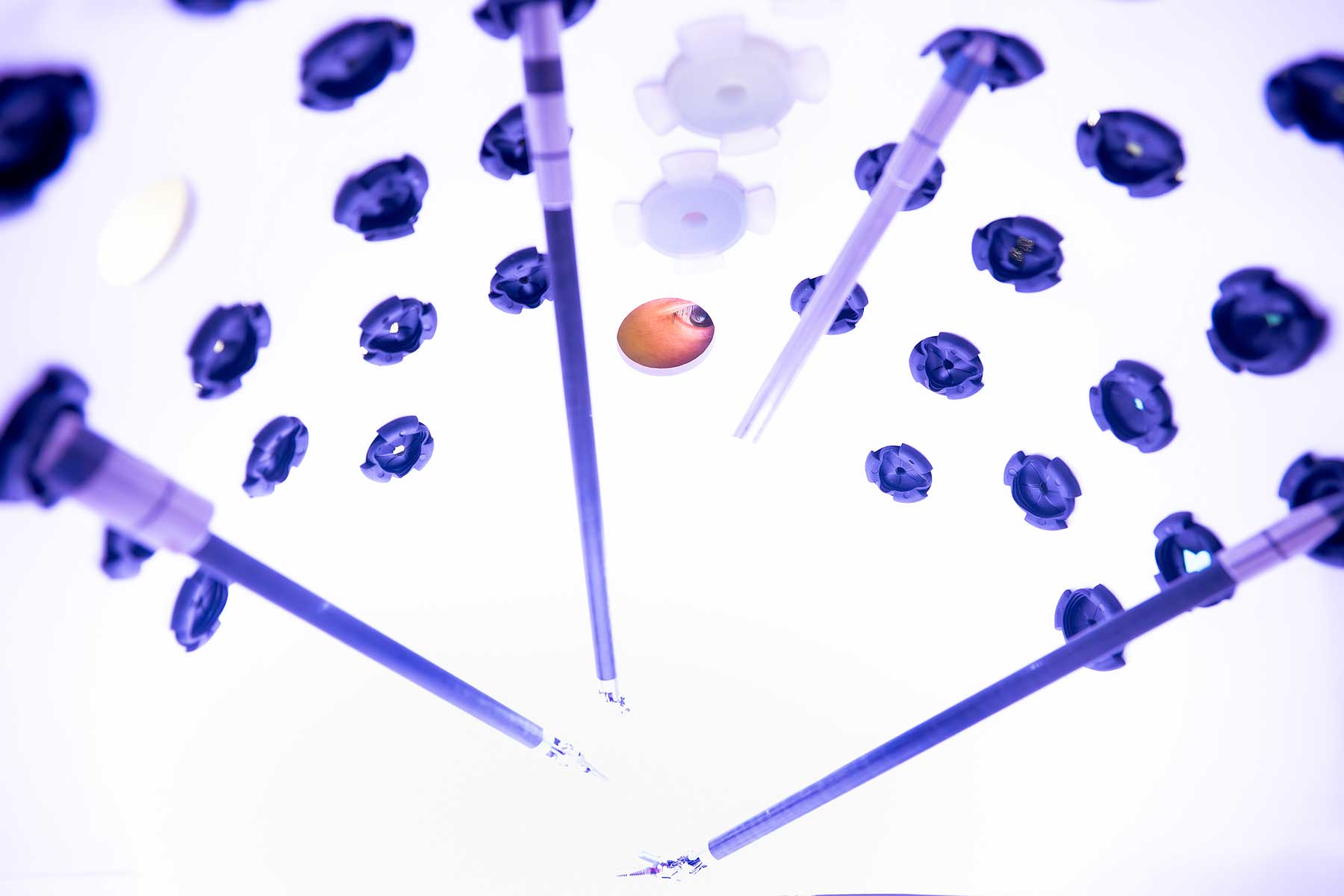
The bedside certification program includes an online introduction to the robot and its array of buttons, arms, and pedals. Next, Gomes and Murillo lead learners in small group hands-on tutorials where they practice manipulating the robot’s arms, switching out arm-mounted tools, and cleaning the camera. Once completed, medical students receive a sticker of a cartoon robot to add to their ID badges, signaling to UCSF operating room staff at its Parnassus and Mission Bay facilities that the learner is a certified assistant.
Although they can begin scrubbing into surgical cases, they’ll be paired with trained bedside assistants for a series of cases before working as the primary bedside assistant. Throughout their time in the operating room, learners receive weekly email check-ins gauging their experiences and providing feedback from the surgeons and teams with whom they worked.
The careful approach balances educational opportunities with patient safety, Gomes explains.
“The nurse managers, the attending physicians, the residents, the bedside staff — they all welcome the students and really enjoy providing a meaningful learning opportunity,” she says. “I’m appreciative of UCSF’s culture for promoting this kind of open-mindedness and allowing students to function in this role as part of their education.”
To residency and beyond
So far, more than a dozen students have become certified bedside assistants. Many learners say it strengthened their interest in robotic surgery and made them more competitive candidates for prestigious residency programs.
Back at the Surgical Skills Lab, medical student and certified bedside assistant Jessica Santhakumar helps the team prepare for an upcoming class, rolling gauze into tiny packets to be used as part of laparoscopy training. From the back of the room, she watches as the new medical interns explore the robot and practice moving its arms.
Santhakumar dreams of working with the surgical device industry as a future surgeon after graduation. She completed her bedside certification in April and has since acted as a bedside assistant in more than a dozen robotic surgeries.
“At first, it was very intimidating, but our instructors warned us that we’d be nervous and encouraged us to try our best and ask for help when we needed it,” she remembers. “I just went up to our scrub nurse and let them know that it was my first or second time assisting and I’d love to learn from them. The whole team set me up for success.”
Santhakumar now scrubs in regularly for surgeries at UCSF Helen Diller Medical Center at Parnassus Heights.
“I’ve been encouraging all my friends applying to general surgery residency to go for this training because it really helps us shine in our rotations,” she adds.
In July, Chern received the country’s highest honor in surgery education for UCSF’s robotic surgery program, having been admitted to the American College of Surgeons Academy of Master Surgeon Educators.
“What’s really beautiful about this work is the input that I, as a student, and other students had into this curriculum because it’s ultimately for students,” Edwards says. “It’s a beautiful example of designing a program with the people it’s intended for.”


