Laura López González, UC San Francisco
Science is a lot like real estate: It’s about location, location, location, said UC San Francisco physiology professor David Julius, Ph.D., on the heels of his 2021 Nobel Prize. For five decades, UC San Francisco has been one of the most sought-after addresses in the world of science and a place where Nobel laureates are born.
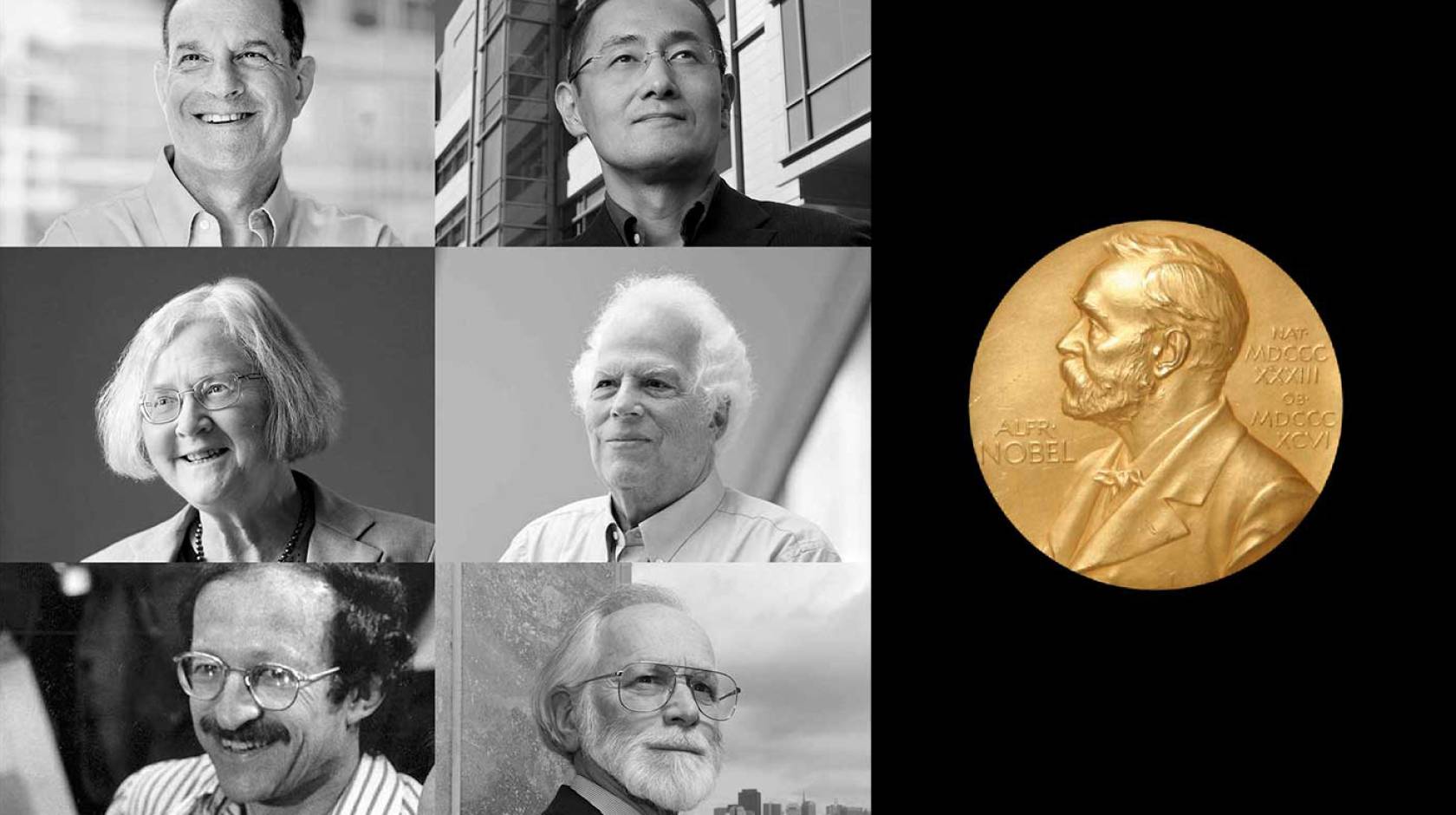
Each year, the Nobel Prize in physiology or medicine is awarded to scientists whose work has irrevocably changed medicine, from discoveries that reveal life’s fundamental mechanisms to life-saving treatments. Since its 1901 inception, 115 Nobel Prizes in physiology or medicine have been awarded to scientists, including six UCSF faculty members. This places UCSF among the top U.S. medical schools for this illustrious medal count.
In conjunction with the 2025 Nobel Prize awards announcements Oct. 6 to 13, we take a look back at the Nobel Prize-winning discoveries that changed the world.
What he discovered
Our ability to sense pain, heat, and touch is fundamental to how we experience the world — shaping everyday interactions to life’s most profound moments. Yet for millennia, the biological mechanisms behind these sensations remained a mystery.
Inspired partly by traditional or “folk” medicine, nature became Julius’ muse. He studied everything from tarantula toxins and coral snake venom to the chemical compound capsaicin, which gives chilies their spice.
By investigating how these substances produce sensations of pain and temperature, Julius discovered how a family of proteins play a central role in the nervous system’s sensory pathways and explains why chili peppers burn, but also how our bodies detect heat, cold, and mechanical pressure.
Why it matters
Julius’ groundbreaking work has reshaped our understanding of pain at the molecular level — laying the foundation for the development of safer, non-addictive future pain treatments.
What he discovered
An embryo has the beginnings of every cell our bodies will ever produce. That’s partly because embryonic stem cells can become almost any kind of cell, like skin, nerve, muscle, or blood cells. This cellular superpower is called pluripotency. But as these stem cells age, this superpower vanishes.
But in 2007, UCSF Anatomy Professor Shinya Yamanaka, M.D., Ph.D., discovered how to turn back time. Surprisingly, by introducing only a few genes, he could reprogram mature cells to return to their pluripotent state. It was a cellular tale seemingly from the pages of American author F. Scott Fitzgerald’s short story, “The Curious Case of Benjamin Button,” in which the tale’s namesake ages in reverse.
Why it matters
Yamanaka’s discovery rewrote textbooks and created new research fields. Today, his work has unlocked new opportunities to study disease, and develop tests and treatments for conditions such as Alzheimer’s, leukemia, and heart disease.
What she discovered
Every human cell holds DNA, which contains the instructions for making proteins responsible for virtually all of the body’s processes, from metabolism to immunity. These genetic instructions are neatly organized into sections called chromosomes. These tightly coiled structures, made of DNA and proteins, must produce exact copies of themselves when cells reproduce, or divide.
Biochemistry and Biophysics Professor Elizabeth Blackburn, PhD, discovered that chromosomes carry tiny end caps called telomeres that protect chromosomes from being broken down.
And a cell’s life, she discovered, is defined by these telomeres in many ways. Telomeres safeguard chromosomes during cell division, ensuring that crucial genetic information is not lost as DNA is copied. When these caps become too short, cells age and lose their ability to reproduce. But if telomeres remain long — as in cancer cells — cells can divide and spread indefinitely.
Why it matters
Blackburn’s work solved a major problem in biology: how chromosomes can be copied in their entirety during cell division. Today, the study of telomeres is a major scientific field advancing work on new cancer therapies and aging.
What he discovered
In the 1950s, scientists classified a rare but deadly disease, Kuru, in Papua New Guinea. Victims developed tremors, weakness, and — bizarrely — fits of uncontrollable laughing before dying. The mystery illness didn’t behave like most illnesses. There were no characteristic signs of infection, for example, no fever or inflammation. Kuru did, however, resemble Creutzfeldt–Jakob disease, a rare fatal brain disorder described in Germany two decades earlier.
In 1982, Neurology Professor Stanley Prusiner, M.D., uncovered what caused these diseases. It wasn’t anything science thought made people ill — it wasn’t a virus, bacteria, parasite, or even a fungus. It was history’s first class of infectious protein, which he dubbed prions.
Prions are a misfolded or misshapen version of a normal protein found in the brain. When prions interact with normal proteins, they cause the normal proteins to fold abnormally too and become prions themselves. Over time, these misfolded proteins accumulate, damaging the brain.
Why it matters
Since Prusiner’s Nobel Prize, UCSF scientists have built on his work, identifying new prions and exploring how prion-like proteins may contribute to more common forms of neurodegeneration, such as Parkinson’s disease and Alzheimer’s disease.
What they discovered
The origins of cancer were unknown when former UCSF Chancellor J. Michael Bishop began his career in the 1960s, until he and his colleague Harold E. Varmus, then a professor of microbiology, biochemistry, and biophysics, unlocked its secrets. It started with the help of a chicken.
Identified at the turn of the 20th century, Rous sarcoma virus gained short-lived notoriety as the first virus ever documented to cause cancer — in chickens, that is. The virus slipped into relative scientific obscurity until UC researchers and others revived the work in the ’60s and ’70s. Soon, UC Berkeley scientists discovered that a single gene from the virus was enough to make cells become cancerous.
Bishop and Varmus were intrigued; the gene was present in cancer cells, obviously, but where did it come from? Could it be in healthy cells too? Samples from quails, ostriches, and even an emu at the San Francisco Zoo all showed similar genes.
Normal cells, the pair found, were capable of becoming cancerous. Cancer wasn’t some invader — these experiments showed — instead, the threat lurked within us. In horror movie terms: The call was coming from inside the house.
Why it matters
The pair’s research proved the existence of oncogenes, mutated genes that cause cancer. The discovery ushered in the era of modern cancer care, paving the way for researchers to identify genes like HER2 as oncogenes for some aggressive breast cancers and to develop specially targeted treatments, such as the well-known drug Herceptin.

